Regardless of the pathogen, the disease has similar symptoms, mechanism of occurrence and treatment tactics. Foot fungus is a common and contagious disease. It is characterized by a high frequency of occurrence in the presence of concomitant conditions and diseases, for example, foci of chronic inflammation, endocrine diseases, decreased immunity and other diseases. As a rule, the disease is chronic in nature with exacerbations in the summer and attenuation of the process (remission) in the winter.
Signs of ringworm
- Color change
- Inflammation
- Appearance of spots
- Erosion
- Deformation and thickening
Types of fungal foot diseases
Depending on the types of fungi that cause the disease, foot mycoses are divided into:
Yeast-like mycoses: caused by fungi of the genus Candida.
Fungal mycoses: caused by the fungi Scytalidium spp. , Onychocola canadensis, Scopulariopsis brevicaulis, Aspergillus, Fusarium, Alternaria, Penicillium.
Dermatomycosis: caused by dermatomycetes of the genera Trichophyton, Epidermophyton. Fungi of this species need keratin to function, which is rich in the stratum corneum of the skin, nails and hair. The group of dermatomycoses with predominant nail lesions includes rubrophytosis (the causative agent isTrichophyton rubrum) and athlete's foot (causative agent - Trichophyton interdigitale). Trichophyton rubrum is responsible for approximately 80-90% of athlete's foot cases.
Mixed mycoses: caused by several types of fungi at the same time.
Each type of ringworm is described in detail below.
Yeast-like mycoses
Recently, foot mycoses caused by fungi of the genus Candida have become widespread. It is assumed that this is due to the widespread use of various medications, the action of which is associated with interaction with the immune system.
Dermatomycoses
Athlete's foot is a chronic disease that is located in the skin of the arches and interdigital folds of the feet, with frequent injuries to the nail plates.
Mold mycoses
Fungal mycoses are common mainly in countries where people traditionally walk barefoot (eastern, subtropical and tropical countries). In regions with a temperate climate, this type of mycosis also occurs, but, as a rule, in patients with immunodeficiency and in people who frequently come into contact with soil and plants.
Forms of foot mycosis
There are several forms of ringworm:
Scaly
It is characterized by peeling of the skin on the arches of the feet, possibly spreading to the surface of the toes. Areas of skin thickening and lamellar peeling may also appear.
Intertriginous
Similar to interdigital diaper rash. The inflammatory process is usually located between the 3rd and 4th fingers. The stratum corneum softens, becomes loose and flakes off. Cracks and a whitish layer appear. Itching and burning begin. It is possible to add pyococcal flora (pustular infection) and yeast, then the affected areas are covered with purulent and bloody crusts.
Dyshidrotic
It is characterized by the appearance on the lateral surface of the feet and on the surfaces of the fingers in contact with them, blisters filled with a transparent liquid and covered by a thick stratum corneum. Sago grains (vesicles) can be single or merge into multi-chambered bubbles. As the pyococci unite, the contents of the vesicles become cloudy, then they open and erosions are formed, covered with purulent-hemorrhagic crusts. Some patients notice inflammation of the lymph nodes and deterioration in general health.
In 2/3 of patients with intertriginous and dyshidrotic forms of epidermophytosis, mycids (allergic skin rash) are observed.
Of course, the identification of clinical forms of epidermophytosis is conditional, since their combination often occurs, one form can transform into another. It all depends on the body's reaction, physical activity and the patient's treatment methods.
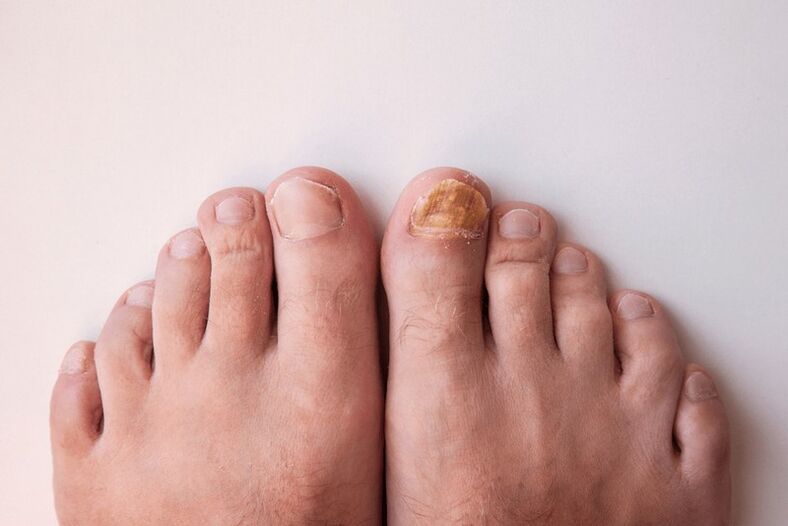
Furthermore, in foot mycosis, the nails are often affected, especially on the first and fifth toes. The nail plate acquires yellowish spots or stripes, the surface becomes dull and uneven, and a horny thickening begins to appear under the nail, which subsequently leads to the destruction of the nail plate.
Watching the corresponding video on the Internet, you can find out that foot fungus can be caused by different factors, and in order to choose the tactics for treating this disease, it is necessary to determine the type of fungus and establish the cause of its appearance.
Causes of foot fungus
The main causes of foot fungus are:
- Excessive sweating or, conversely, increased dryness and peeling of the feet. These processes disrupt the protective function of skin cells.
- Anatomical features: narrow spaces between the toes and their deformation, flat feet.
- Problems with thermoregulation (maintenance of a certain body temperature) and microcirculation (transport of biological fluids).
- Wounds, injuries that violate the integrity of the skin. Through these injuries, infections often occur.
- The presence of diseases that reduce immunity or lead to metabolic disorders (for example, endocrinopathies, blood diseases, oncology, etc. ).
- Taking certain medications (antibacterials, cytostatics, corticosteroids).
Often, fungal infections of the feet are combined with pustular rashes, so assumptions are made about the relationship between them: thanks to pyococci, dermatophytes penetrate deep into the subcutaneous tissue, and prolonged mycoses due to the formation of cracks, scratches and erosions contribute to the increase susceptibility to infection.
Often with foot fungus a viral infection occurs. For example, the causative agent of rubromycosis activates papillomavirus and herpes virus. This manifests itself in an increased concentration of viruses on the surface of fungal-infected cells.
The source of the spread of the disease is people suffering from ringworm: during the peeling process, skin flakes containing the pathogens of the fungal infection are highlighted. These infected scales often end up on the floor and on pool equipment, bathtubs, and pedicure tools.
An interesting fact is that mushrooms are highly resistant and can be stored in hot springs, chlorinated and ozonated water for 12 to 18 days. Water with a high salt or hydrogen sulfide content is harmful to fungi.
Therefore, we must remember that the general mechanisms contributing to the development of fungal infections on the feet are caused by a violation of the body's natural resistance, changes in immunological and metabolic processes.
Diagnosis of foot fungus
Diagnosis of foot fungus includes:
- Assess patient complaints and the presence of chronic diseases.
- Microscopic examination of affected skin and nail particles.
- Cultural sowing is the placement of pathogenic microorganisms in a nutrient medium for their reproduction and subsequent accurate identification, as well as to evaluate the activity of antifungal drugs and determine the sensitivity of fungi to them.
To select the appropriate therapy, it is important to determine whether the changes in the skin of the foot are a fungal infection or dyshidrotic eczema, keratoderma, psoriasis and other skin diseases.
Antifungal medicines, agents, antimycotics
Antifungal agents: classification and types of pharmaceutical forms. Methods of using antimycotics.
Foot fungus treatment
Treatment of foot fungus must be carried out comprehensively, it is important not only to suppress the proliferation of pathogenic microorganisms and eliminate symptoms, but also to destroy pathogens and eliminate the cause of their occurrence (increase immunity, immediately treat small wounds on the feet, etc. ). It is imperative to treat concomitant diseases that cause the development of fungal infections.
Additionally, some people may have allergic reactions to certain mushrooms (such as mykids). In these cases, antihistamine (antiallergic) medications may be necessary.
To treat mycoses, as a rule, topical preparations are used, that is, those that are applied directly to the affected area of the skin. These products are produced in the form of ointments, creams, sprays, solutions and varnishes (for nails).
Depending on the mechanism of action, antifungal agents can have a fungistatic effect, inhibiting the growth and reproduction of fungi, or they can have a fungicidal effect and promote the death of fungi.
As foot mycoses are most often caused by a mixed fungal flora, it is more effective to use broad-spectrum agents. This includes medications that have their own anti-inflammatory and antipruritic effects.
The use of special purpose products in the treatment of foot fungus
Modern antimycotic drugs are highly effective against pathogenic fungi of the genus Candida, dermatophytes (Trichophyton, Microsporum) and other causative agents of skin infections, gram-positive strains of staphylococci and streptococci. They block the growth and reproduction of fungi (fungistatic effect), destroy fungi (fungicide effect) when used in therapeutic doses, have their own anti-inflammatory and antipruritic effect
















